Prescription trends
In the United Kingdom the use of antidepressants increased by 234% in the 10
years up to 2002.
In the United States a 2005 independent report stated that 11% of women and 5%
of men in the non-institutionalized population (2002) now take antidepressants
A 1998 survey found that 67% of patients diagnosed with depression were
prescribed an antidepressant.
A 2007 study purports that 25% of Americans were overdiagnosed with depression,
regardless of any medical intervention.
The findings were based on a national survey of 8,098 people.
A 2002 survey found that about 3.5% of all people in
rance were
being prescribed antidepressants, compared to 1.7% in 1992, often for conditions
other than depression and often not in line with authorizations or guidelines
Between 1996 and 2004 in
British Columbia, antidepressant use increased from 3.4% to 7.2% of the
population
Data from 1992 to 2001 from the
Netherlands indicated an increasing rate of prescriptions of SSRIs, and an
increasing duration of treatment.
Surveys indicate that antidepressant use, particularly of SSRIs, has
increased rapidly in most developed countries, driven by an increased awareness
of depression together with the availability and commercial promotion of new
antidepressants.
Antidepressants are also increasingly used worldwide for non-depressive patients
as studies continue to show the potential of immunomodulatory, analgesic and
anti-inflammatory properties in antidepressants.
The choice of particular antidepressant is reported to be based, in the
absence of research evidence of differences in efficacy, on seeking to avoid
certain side effects, and taking into account comorbid (co-occurring)
psychiatric disorders, specific clinical symptoms and prior treatment history
It is also reported that, despite equivocal evidence of a significant
difference in efficacy between older and newer antidepressants, clinicians
perceive the newer drugs, including SSRIs and SNRIs, to be more effective than
the older drugs (tricyclics and MAOIs).
A survey in the UK found that male general physicians were more likely to
prescribe antidepressants than female doctors.
Most commonly prescribed antidepressants
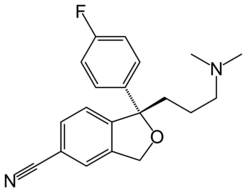
Structural formula of the SSRI
escitalopram, in its free base form.
The most commonly prescribed antidepressants in the US retail market in 2006
were:
-
Sertraline (Zoloft) - of the
SSRI class, with 28.060 million prescriptions
-
Escitalopram (Lexapro) - of the
SSRI class, with 26.098 million prescriptions
-
Fluoxetine (Prozac) - of the
SSRI class, with 21.733 million prescriptions
-
Bupropion (Wellbutrin, Zyban) - of the
NDRI class, with 21.141 million prescriptions
-
Paroxetine (Paxil) - of the
SSRI class, with 19.472 million prescriptions
-
Venlafaxine (Effexor) - of the
NRI class,
with 17.101 million prescriptions
-
Trazodone (Desyrel), with 14.628 million prescriptions
-
Amitriptyline (Elavil), with 13.924 million prescriptions
-
Citalopram (Celexa), of the
SSRI class, with 11.986 million prescriptions
-
Duloxetine (Cymbalta), of the
NRI class,
with 8.520 million prescriptions
-
Mirtazapine (Remeron), with 4.852 million prescriptions
-
Nortriptyline (Pamelor), with 3.174 million prescriptions
-
Imipramine (Tofranil), with 1.629 million prescriptions
The most commonly prescribed antidepressant in Germany is reported to be
(concentrated extracts of) hypericum perforatum (St John's Wort).
[13] In the Netherlands, paroxetine, marketed as Seroxat among generic
preparations, is the most prescribed antidepressant, followed by the tricyclic
antidepressant amitriptyline, citalopram and venlafaxine.
[14]
Mechanisms of action
The therapeutic effects of antidepressants are believed to be related to
their effects on
neurotransmitters.
Monoamine oxidase inhibitors (MAOIs) block the break-down of monoamine
neurotransmitters (erotonin
and
norepinephrine) by inhibiting the
nzymes which
oxidize them, thus leaving higher levels still active in the brain (ynaptic
cleft).
Tricyclic antidepressants (TCAs) prevent the reuptake of various
neurotransmitters, including
erotonin,
norepinephrine, and
opamine.
Selective serotonin reuptake inhibitors (SSRIs) more specifically prevent
the reuptake of serotonin (thereby increasing the level of active serotonin in
synapses of the
brain). Other novel antidepressants specifically affect serotonin and other
neurotransmitters.
A theory centered on neurotransmitter effects appears to be incomplete,
however. Neurotransmitter levels are altered as soon as the antidepressant
chemicals build up in the bloodstream, but effects on mood appear to occur
several days or weeks later.
One explanation of this holds that the "own-regulation"
of neurotransmitter
receptors�an apparent consequence of excess signaling and a process that
takes several weeks�is actually the mechanism responsible for the alleviation of
depressive symptoms. Another hypothesis is that antidepressants may have some
longer-term effects due to the promotion of
neurogenesis in the
hippocampus, an effect found in mice
Other animal research suggests that antidepressants can also affect the
expression of genes in brain cells, by influencing "lock
genes".
New research suggests that delayed onset of clinical effects from
antidepressants indicates involvement of adaptive changes in antidepressant
effects. Rodent studies have consistently shown upregulation of the
3, 5-cyclic adenosine monophosphate (cAMP) system induced by different types
of chronic but not acute antidepressant treatment including serotonin and
norepinephrine uptake inhibitors, monoamine oxidase inhibitors, tricyclic
antidepressants, lithium and electroconvulsions. cAMP is synthesized from
adenosine 5-triphosphate (ATP) by adenylyl cyclase and metabolized by cyclic
nucleotide
phosphodiesterases (PDEs).
Data also suggest antidepressants to have the ability of modulating
neural plasticity in longterm administration.
Anti-inflammatory and immunomodulation Recent studies show pro-inflammatory
ytokine
processes take place during
depression, ania
and
bipolar disease, and is possible that symptoms manifest in these psychiatric
illnesses are being attenuated by pharmacological affect of antidepressants on
the immune system.
Studies also show that the chronic secretion of
stress
hormones as a result of disease, including
somatic
infections or
autoimmune syndromes may reduce the effect of
neurotransmitters or other receptors in the brain by
cell-mediated pro-inflammatory pathways, thereby leading to the
dysregulation of neurohormones.
SSRIs, NRIs
and
tricyclic
antidepressants acting on
erotonin,
norepinephrine and
opamine
receptors have been shown to be immunomodulatory and anti-inflammatory against
pro-inflammatory
ytokine
processes, specifically on the regulation of
Interferon-gamma (IFN-gamma) and
Interleukin-10 (IL-10), as well as
TNF-alpha and
Interleukin-6 (IL-6). Antidepressants have also been shown to suppress
H1
upregulation.
Antidepressants, specifically TCAs and dual serotonergic-noradrenergic
reuptake inhibition by dual SNRIs (or SSRI-NRI combinations), have also shown
nalgesic
properties.
These studies warrant investigation for antidepressants for use in both
psychiatric and non-psychiatric illness and that a
psycho-neuroimmunological approach may be required for optimal
pharmacotherapy.
Future antidepressants may be made to specifically target the immune system by
either blocking the actions of pro-inflammatory cytokines or increasing the
production of anti-inflammatory cytokines.
|

