Local anesthetic agents and their history
Surprisingly, the first local anesthetic was Cocaine which was
isolated from coca leaves by Albert Niemann in Germany in the 1860s. The very
first clinical use of Cocaine was in 1884 by (of all people) Sigmund Freud who
used it to wean a patient from morphine addiction. It was Freud and his
colleague Karl Kollar who first
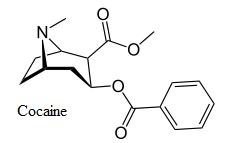 noticed
its anesthetic effect. Kollar first introduced it to clinical ophthalmology as
a topical ocular (eye) anesthetic. Also in 1884, Dr. William Stewart Halsted
was the first to describe the injection of cocaine into a sensory nerve trunk to
create surgical anesthesia. Halsted was an eminent surgeon who had been trained
in Britain. He was the first to establish formal surgical training for
physicians in America. Prior to that time, surgery was a self taught discipline
among US physicians. He also invented and pioneered the use of rubber gloves.
Unfortunately, much to his own regret, he began to use cocaine himself and
became highly addicted to it. At that time, there was no stigma attached to the
recreational use of cocaine, and it gained a following among the elites of the
day. Arthur Conan Doyle's Sherlock Holmes was supposed to be an addict, and
Holmes kept Dr Watson around as a source for his drugs, as well as for the comic
relief he provided.
noticed
its anesthetic effect. Kollar first introduced it to clinical ophthalmology as
a topical ocular (eye) anesthetic. Also in 1884, Dr. William Stewart Halsted
was the first to describe the injection of cocaine into a sensory nerve trunk to
create surgical anesthesia. Halsted was an eminent surgeon who had been trained
in Britain. He was the first to establish formal surgical training for
physicians in America. Prior to that time, surgery was a self taught discipline
among US physicians. He also invented and pioneered the use of rubber gloves.
Unfortunately, much to his own regret, he began to use cocaine himself and
became highly addicted to it. At that time, there was no stigma attached to the
recreational use of cocaine, and it gained a following among the elites of the
day. Arthur Conan Doyle's Sherlock Holmes was supposed to be an addict, and
Holmes kept Dr Watson around as a source for his drugs, as well as for the comic
relief he provided.
It became fairly obvious fairly quickly that while the
anesthetic characteristics of cocaine were desirable, the euphoria and
subsequent addiction it produced were not! The turn of the century was a
tremendous time of scientific progress, and the new discipline of
 organic
chemistry enabled the synthesis of the first analog of cocaine in 1905. (An
analog of a chemical molecule is one in which the original molecule is
progressively modified to retain and enhance certain holistic characteristics of
the original substance while ridding it of other unwanted characteristics.) The
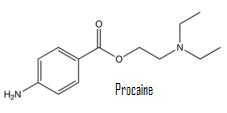
first synthetic local anesthetic was procaine, better remembered today by
its trade name, "Novocain".
organic
chemistry enabled the synthesis of the first analog of cocaine in 1905. (An
analog of a chemical molecule is one in which the original molecule is
progressively modified to retain and enhance certain holistic characteristics of
the original substance while ridding it of other unwanted characteristics.) The
first synthetic local anesthetic was procaine, better remembered today by
its trade name, "Novocain".
Novocain was not without its problems. It took a very long time
to set (ie. to produce the desired anesthetic result), wore off too quickly and
was not nearly as potent as cocaine. On top of that, it is classified as an
ester. Esters have a very high potential to cause allergic reactions. It is
estimated that about one third of all persons who received it developed at least
minor allergic reactions to it. Faced with the legal and ethical difficulties
associated with the use of cocaine as a local anesthetic, and with the
inefficiencies and allergenicity associated with the use of procaine, it is not
surprising that most dentists of the day worked without any local anesthetic at
all. (Nitrous oxide gas was available during this period.) Today, procaine is
not even available for dental procedures.
| In 1942, W.C. Fields made a movie called "The dentist". It was
a bawdy, slapstick comedy short (25 minutes) which included scenes
of Fields as a dentist working on patients, complete with the sound
of a buzz saw. It was, of course, meant to be funny, but it shows a
patient squirming in the dental chair, and in this sense, at least,
was probably not far from the truth about dentistry up until shortly
after the film was made. You can download a clip from the film
here. (The link to the clip is near
the bottom of the page) |
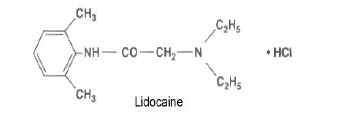 The
first modern local anesthetic agent was lidocaine (trade name
Xylocaine�). It was invented in the 1940s. Prior to its introduction,
Nitrous oxide gas and procaine (plus alcohol in the form of whiskey) were the
major sources of pain relief during dental procedures. Lidocaine proved to be
so successful that during the 1940s and 1950s the use of procaine and nitrous
oxide gas as primary anesthetic agents all but vanished. (Whiskey somehow
survived, but it is no longer used on patients.) Today, nitrous oxide is
used principally as an anti-anxiety palliative, and Novocaine is no longer
available.
The
first modern local anesthetic agent was lidocaine (trade name
Xylocaine�). It was invented in the 1940s. Prior to its introduction,
Nitrous oxide gas and procaine (plus alcohol in the form of whiskey) were the
major sources of pain relief during dental procedures. Lidocaine proved to be
so successful that during the 1940s and 1950s the use of procaine and nitrous
oxide gas as primary anesthetic agents all but vanished. (Whiskey somehow
survived, but it is no longer used on patients.) Today, nitrous oxide is
used principally as an anti-anxiety palliative, and Novocaine is no longer
available.
Lidocaine (along with all other injectable anesthetics
used in modern dentistry) is in a broad class of chemicals called amides, and
unlike ester based anesthetics, amides are hypoallergenic. It sets
quickly and when combined with a small amount of
epinephrine (adrenalin), it produces
profound anesthesia for several hours. Lidocaine is still the most widely used
local anesthetic in America today.
Over the next thirty years, a number of other amide local
anesthetics were invented, most not differing significantly from lidocaine. The
major problem with lidocaine and its analogs is that they cause vasodilation,
or the tendency of the local blood vessels to open wider increasing the blood
flow in the area. This causes the anesthetic to be absorbed too quickly to take
effect. Hence these anesthetics are always mixed with low concentrations of
epinephrine which has the opposite effect (ie vasoconstriction) and
closes the blood vessels down to keep the anesthesia in position long enough to
produce long lasting numbness.
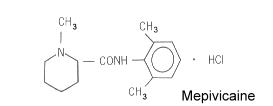 Mepivicaine
(Carbocaine�) and prilocaine (Citanest�)
have much less vasodilative qualities and hence can be used without the
epinephrine vasoconstrictor. The advantage to this is that these anesthetics
can be used more safely in patients who are taking medications which may
interact negatively with the vasoconstrictor. These drugs include certain blood
pressure medications (most notably non selective beta blockers) and tricyclic
antidepressants (Elevil� and imipramine are two examples). Carpules that do
not contain the vasoconstrictor also do not contain a preservative. This
eliminates a possible source of allergic reaction.
Mepivicaine
(Carbocaine�) and prilocaine (Citanest�)
have much less vasodilative qualities and hence can be used without the
epinephrine vasoconstrictor. The advantage to this is that these anesthetics
can be used more safely in patients who are taking medications which may
interact negatively with the vasoconstrictor. These drugs include certain blood
pressure medications (most notably non selective beta blockers) and tricyclic
antidepressants (Elevil� and imipramine are two examples). Carpules that do
not contain the vasoconstrictor also do not contain a preservative. This
eliminates a possible source of allergic reaction.
Bupivicaine (Marcaine�)
Bupivicaine is a special case in dental anesthesia. It is used
mostly by surgeons who want to produce very long acting anesthetic effects in
order to delay the post operative pain from their surgery for as long as
possible. Bupivicaine comes in 0.5% solution with a vasoconstrictor. It is the
most toxic of all the anesthetic agents and this toxicity is reflected in its
low concentration in the carpules. As noted in the
PKa table, it is has a very alkaline (basic)
PKa which means that a relatively low percentage of the uncharged base radical
(RN) is available for immediate diffusion through the
cell membrane. Thus it takes a fairly long
time to set. However, once inside the cell membrane, over 80% of the radicals
that do diffuse become available for binding to the sodium channel proteins.
This high protein binding ability causes the drug to remain active for a long
time once it has diffused through the cell membrane. (PKa and its relationship
with cell membrane permeability is a concept explained
later in this course.)
 Prilocaine
(Citanest�)
Prilocaine
(Citanest�)
Prilocaine has the same general
PKa as lidocaine, which means that for all
practical purposes it can be used in the same way and at the same concentrations
as lidocaine, producing about the same anesthetic affect in the same setting
time for the same duration. It is, however somewhat
less toxic in higher doses than lidocaine, and
thus is delivered in a 4% solution which places about twice as much molecular
anesthetic in proximity to the nerve as is the case with lidocaine or
mepivicaine. In addition, since it has little vasodilatory activity, it may be
used without a
vasoconstrictor. The higher concentration of
anesthetic agent, in combination with a vasoconstrictor, therefore, gives this
anesthetic the twin advantages of fast onset of activity with prolonged
anesthetic activity due to the larger number of molecules available to cross the
cell membrane. Unfortunately, the toxicity of a single carpule of 4% prilocaine
is still greater than the toxicity of a single carpule of 2% lidocaine which
means that fewer carpules can be used before toxic levels are reached. Higher
toxicity translates into a higher likelihood of prolonged or permanent
paresthesia or anesthesia after using this drug for major nerve blocks.
Articaine (Septocaine�)
Articaine is the newest addition to the local anesthetic arsenal
and was approved by the Food and Drug Administration in April 2000. It has been
in use in Europe since 1976 and in Canada since 1983. Its approval in the US
has been delayed by the FDA due to the presence of a preservative which the
agency said was unnecessary in single use carpules and was a potential allergen.
It was approved when the French company Septodent finally removed the
preservative from American shipments.
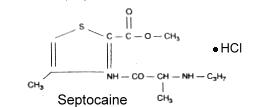 Articaine
has the same
PKa and toxicity as Lidocaine, however it is
metabolized differently. It has a half life in the body less than 1/4 as long
as that of lidocaine and only 1/5 as long as mepivicaine. This means that more
of the drug can be injected later in the dental procedure with less likelihood
of blood concentrations building to toxic levels. Articaine is formulated in a
4.0% solution with
vasoconstrictor. The presence of the
vasoconstrictor retards the systemic absorption of the anesthetic allowing
higher concentrations of the drug to remain in the area of injection and slowing
the absorption into the bloodstream. The higher local concentration of the drug
produces a high level of the uncharged radical (RN) to be present at the
membrane which brings about very rapid absorption of the drug. (The concept of
membrane permeability is discussed on
page 4 in this course.) In addition, the
benzene ring on the left end of the molecule has been replaced with a thiophene
ring. This modification allows for faster and more complete absorption through
the nerve cell membrane. The ability of this drug to penetrate barriers is so
great that it has been used to penetrate thick bone to produce anesthesia in a
way that other anesthetics cannot. Articaine has become the local anesthetic of
choice in most countries into which it has been introduced. I have found that
it produces profound anesthesia (in most patients) when used as an infiltration
(field block) for mandibular premolars and anterior teeth instead of the
traditional mandibular nerve block..
Articaine
has the same
PKa and toxicity as Lidocaine, however it is
metabolized differently. It has a half life in the body less than 1/4 as long
as that of lidocaine and only 1/5 as long as mepivicaine. This means that more
of the drug can be injected later in the dental procedure with less likelihood
of blood concentrations building to toxic levels. Articaine is formulated in a
4.0% solution with
vasoconstrictor. The presence of the
vasoconstrictor retards the systemic absorption of the anesthetic allowing
higher concentrations of the drug to remain in the area of injection and slowing
the absorption into the bloodstream. The higher local concentration of the drug
produces a high level of the uncharged radical (RN) to be present at the
membrane which brings about very rapid absorption of the drug. (The concept of
membrane permeability is discussed on
page 4 in this course.) In addition, the
benzene ring on the left end of the molecule has been replaced with a thiophene
ring. This modification allows for faster and more complete absorption through
the nerve cell membrane. The ability of this drug to penetrate barriers is so
great that it has been used to penetrate thick bone to produce anesthesia in a
way that other anesthetics cannot. Articaine has become the local anesthetic of
choice in most countries into which it has been introduced. I have found that
it produces profound anesthesia (in most patients) when used as an infiltration
(field block) for mandibular premolars and anterior teeth instead of the
traditional mandibular nerve block..
With clinical reports of profound anesthesia, fast onset, and
success in difficult-to-anesthetize patients, Septocaine has become the most
used dental anesthetic brand name in the US, although lidocaine still remains
the most used type of anesthetic. Recently, the same articaine formulation
became available from a second company under the name Cook-Waite Zorcaine.
Because of its bone penetrating ability, articaine has become
popular for producing profound anesthesia in lower premolars and lower anterior
teeth using localized field blocks (infiltrations) without resorting to
mandibular blocks.
Articaine and prolonged numbness and
paresthesia
Unfortunately, one complication concerning the use of
articaine has arisen. There have been persistent reports of unexplained
paresthesia (burning, tingling, ans sometimes sharp shooting pains in
tissues previously anesthetized with this anesthetic) in a low
percentage of patients. This effect has been noted only when articaine is
used in
major nerve blocks such as the mandibular
block. It has not been noted in
field blocks. So far, no common factor has
been found to explain the link between articaine and persistent paresthesia,
however the higher concentration of anesthetic molecules in the anesthetic
solution (4% for articaine instead of 2% for lidocaine or 3% for mepivicaine
without vasoconstrictor) probably is a factor. The statistics produced for
this phenomenon so far have been quite inconsistent. The incidence for
persistent paresthesia have ranged between 1 in 5,286 for 2002 to 1 in
45,900 in 2004. The incidence for persistent paresthesia for other types of
dental local anesthetic solutions ranged between 1 in 25,850 to 1 in 68,675
during the same timeframe (all statistics approximate; CRA June 2005; vol
29, issue 6).
-
10% of cases of paresthesia lasted for 24 hours or less.
-
52% of cases of paresthesia lasted 1 to 4 weeks.
-
29% of cases of paresthesia lasted 1 month to 1 year.
-
10% of cases of paresthesia lasted for over a year.
-
The most common link with articaine and paresthesia was
administration of mandibular nerve block injections. For this
reason a number of dentists have abandoned the use of articaine for
mandibular nerve blocks, but still use it for infilatration anesthesia
(field blocks) of mandibular anterior teeth and bicuspids.
Treatment of anesthesia and paresthesia
I am not aware of any specific way to treat the numbness
caused by Articaine (other than waiting out the effect), however the
disruptive and often painful paresthesia, including the shooting pains in
the distribution of the affected nerves may be controlled with certain anti
convulsant drugs. One such drug is Lyrica (Pregabalin) 50 mg. three
times a day. Two older drugs in this category are Neurontin (gabapentin)
and Tegretol (carbamazepine).

